Posted on : 10/05/2022 Views : 1812
Joint Preservation: How to avoid and delay joint replacement
Joint replacement especially knee replacement is one of the most common orthopaedic procedures happening in India. Over 100,000 knee replacements are being done every year in our country. In 98.5% of these cases the primary reason for knee replacement is osteoarthritis.

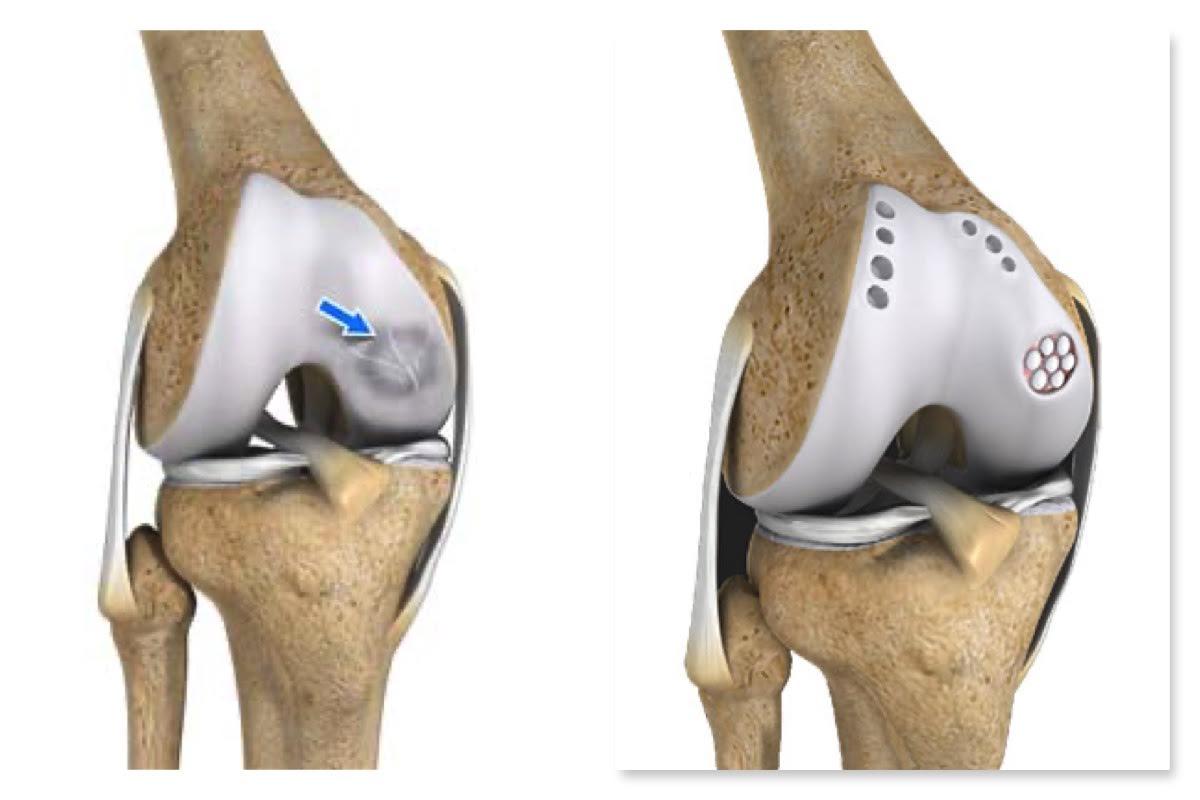
The mechanics and science of joint replacement has come a long way in the past 2 decades. With the advent of advanced instrumentation, minimally invasive techniques and durable light weight alloys, the success rate of joint replacement has improved significantly. Despite this, knee replacement brings along significant morbidity and complications with it, most notable of those being residual knee pain post-surgery and post-operative infection.
Traditionally Knee replacement is considered as a last resort to address the patients knee problem. i.e. knee replacement is only considered as an option when every other procedure to manage the knee issue is pursued and exhausted. Today I would like to talk about these procedures which are employed to delay/avoid, joint replacement. These are broadly called as Joint preservation procedures.
By definition, any surgical procedure that is designed to delay the inevitable joint replacement is called joint preservation procedure. In other words, these procedures prevent the advent of early osteoarthritis or delay its progression into advanced stage.
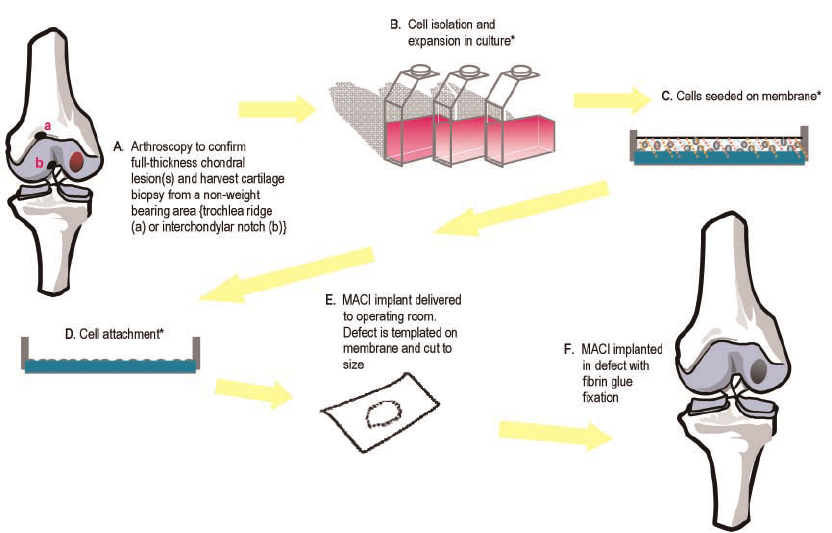
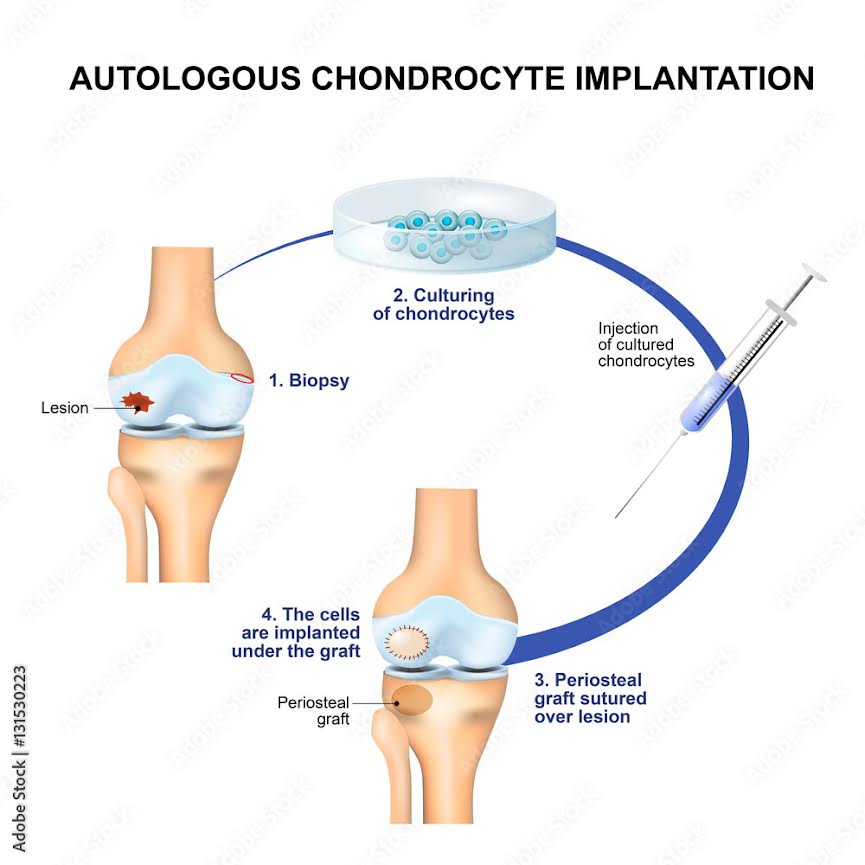
There are four major conditions of the knee that are proven to aggravate the process of osteoarthritis, meniscal insufficiency, ligament injury, chondral damage, malalignment.
Often these conditions may coexist in a subject making the situation complicated. Presence of one or more of these conditions will eventually hasten the process of osteoarthritis for which joint replacement is the only course of action.
Although these conditions may coexist often one will be the primary cause. Careful and meticulous evaluation of the conditions is necessary to determine the order and course of management. All these conditions maybe managed arthroscopically except malalignment which requires osteotomies (fracturing and repositioning of long bones of leg). Given the minimal invasiveness and low impact nature of arthroscopic procedures, the time taken to recover from these surgeries is quite short and ‘return to work’ often happens with in 2-3 weeks after surgery.
Given the natural course of these disorders is osteoarthritis which requires a major surgery in the form of joint replacement, these arthroscopic surgeries to correct these conditions in their initial phase helps to preserve the natural joint. These are the classical ‘stitch in time saves nine’ kind of surgeries.
Although, Joint replacement has come long way and the success rate of joint replacement is close to 98%, every implant that is used has a life span, meaning, there comes a time after joint replacement when the in-situ implant can no longer function or gives away which should be followed by much more complex revision replacement. Hence the native joints should be preserved for as long as possible and joint preservation surgeries are the best options for the purpose.
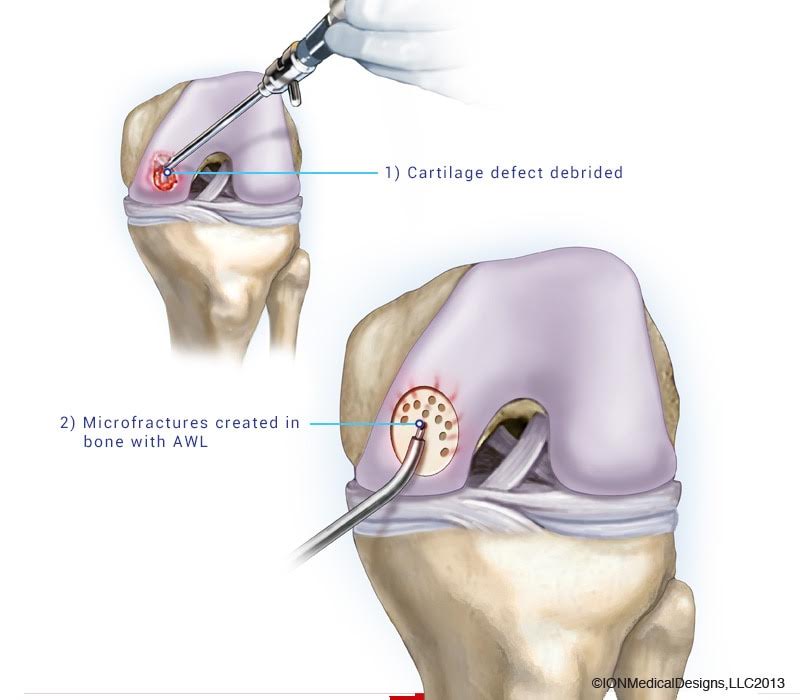
Any review about a surgical procedure is incomplete unless the complications and success rates of the procedure are discussed. The joint preservation procedures are almost always done arthroscopically. These Arthroscopic procedures have a very high success rate of about 95%. Even though the complication rates are negligeable compared to open procedures there are still some incidences of complications. Most common of those being post-operative infection, longer time to regain the range of motion, iatrogenic cartilage injury, portal infection etc. It should be noted that the complication rates of arthroscopic procedures are significantly lower than that of open procedures in the hands of a skilled orthopaedic surgeon.

 (+91) 7022316664
(+91) 7022316664  Emergency: (+91) 80 4566 6616
Emergency: (+91) 80 4566 6616